Treatments
Disorders of the hip
There are many diseases of the hip that can cause symptoms. The most important of these is osteoarthritis, also known as wear and tear. Other causes of hip complaints are femoral head necrosis, or congenital defects such as hip dysplasia. In osteoarthritis, which is most common, the joint is diseased, causing the cartilage, which is the soft sliding layer that covers the bone in the joint, to become thinner and thinner. Unfortunately, there is no good treatment for osteoarthritis, except that painkillers (paracetamol, and then a so-called NSAID added) and lots of exercise, e.g. under the guidance of the physio or exercise therapist, can greatly reduce the symptoms. Patients can really keep their symptoms well under control for a long period of time. It is really wise to give this so-called “conservative” treatment of osteoarthritis a good try first before considering the placement of an artificial hip joint. Also because there are quite a few risks involved in its placement. During a visit to the outpatient clinic, this will be explained to you in detail. There are also age-related and personal aspects to this.
Total hip replacement (artificial hip)
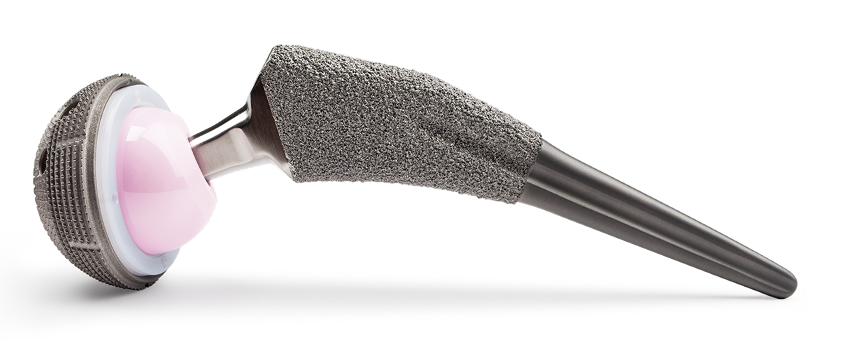
When placing a total hip replacement, the hip head is first removed, and a socket made of titanium and polyethylene (high-quality plastic) is placed in the pelvis. After this, a pin made of titanium or cobalt-chromium is inserted into the femur on which a ceramic head, usually 32 mm in diameter, is placed. There are two ways of securing the prosthesis, with bone glue (cemented) or clamped (uncemented). In patients with good bone quality, an uncemented prosthesis is often chosen.
It is good to know that an artificial hip has a limited lifespan. Much shorter in young people than in older patients. This is mainly because young people use the hip much more and more intensively than older people. In this respect, the hip can well be compared to a car. If you drive it a lot of kilometres, it breaks down sooner. This is also why an artificial hip lasts between 10 and (exceptionally sometimes) 30 years, depending on a patient’s age and activities.
Complications after total hip replacement
Things can go wrong for a shorter or longer period of time after artificial hip placement. Every effort is made to prevent this, but we know that despite all our precautions and careful placement, it sometimes happens.
Infection
Bacteria can get attached to the artificial hip. This can be during the operation, but also in the period afterwards. We do everything possible during surgery to prevent this, but despite this, we know that in a very small number of cases it still happens. If it happens, patients sometimes spend weeks in hospital, multiple surgeries and long-term antibiotics follow, and in the worst case, the prosthesis has to be taken out temporarily or permanently.
Hip dislocation
In the anterior approach, the risk of dislocation of the prosthesis is reduced compared to the posterior approach. Moreover, X-ray monitoring during surgery or robotic arm-assisted placement of the prosthesis reduces the risk even more. Ultimately, however, the risk of dislocation rate of the anterior hip approach is not zero.
Fracture (fracture) of the bone around the prosthesis, loosening or displacement of the prosthesis.
A fracture may occur in the bone around the prosthesis, leading to a longer recovery period or re-operation. Also, the prosthesis may collapse or move and, finally, the prosthesis may become loose after a shorter or longer period of time, which then necessitates a re-operation.
Leg length discrepancy
After surgery, the leg may be slightly longer or shorter than the other leg. Every effort is made to prevent this. For example, you will always be operated using X-rays or a robotic arm to reduce this risk. Nevertheless, slight differences may occur. What you should take into account is that before surgery the leg in most patients was slightly shorter than the other leg. The cartilage layer that is about 1 cm thick in a healthy joint has often completely disappeared in a joint with osteoarthritis. After surgery, the leg therefore often feels 1 cm longer while the legs are actually the same length. For this reason, do not have insoles fitted after surgery, and wait at least until 6 months after surgery and only after consultation with you surgeon.
Blood clot or thrombosis
After surgery, a blood clot may develop in your blood vessels (thrombosis). This can lead to a deep vein thrombosis, a pulmonary embolism and even an infarction. It can therefore have very serious consequences. It is important that you carefully take your medication to prevent a blood clot in the four weeks after surgery.
Blood vessel and nerve damage
Blood vessels may be damaged during surgery. After surgery, this may result in a large hemorrhage. The body often clears this bruise on its own without further consequences. For the first two weeks after surgery, it is helpful to lie on bed with your legs raised for about an hour and a half after lunch to ensure that the leg does not become too swollen.
Nerves may also be damaged during surgery. This may cause the leg or skin or part of it to become numb or paralysed. This is a very rare complication, although it is more common for a small skin nerve to be hit in the operation area. Often other nerves take over, but this can take months to a year.
The main nerve that can be damaged (often temporarily) in the anterior approach is the LFCN. Among other things, this nerve is responsible for sensation of the skin on the outside of the upper leg. Actually, this nerve almost always recovers in the months after surgery. In the so-called Bikini incision (transverse incision in the groin crease), this nerve is more likely to be damaged.
Recovery after total hip replacement
The speed of recovery varies greatly between patients and is difficult to asses prior to surgery. It depends, for example, on the duration and severity of symptoms. It is certainly not the case that patients who are younger or relatively fit do better than older or less fit patients. Indeed, older patients often do better, mainly because they are less likely to make higher demands on the joint. Nor is it the case that extensive exercising after surgery speeds up recovery. Instead, this usually leads to injuries that can be very persistent and take a long time to recover from. Therefor, really don’t do any strength exercises for the first 6-8 weeks after surgery. Give your body and the muscles around the hip joint time to find a new balance and focus on your activities of daily living. Don’t focus on doing exercises, just go for a walk and alternate activities well with taking adequate rest.
Often, patients who are more patient also do better than those who think they can influence their recovery. For recovery after total hip replacement surgery, “haste is seldom good” really applies.

Anterior hip approach
Since 2007, Stephan Vehmeijer has been placing total hip replacements through the anterior approach. This is a technique that causes less damage to surrounding tissues than other approaches to the hip, such as the posterior approach. Actually, the anterior approach to the hip is a very old approach. It was first described in 1881 by Professor Carl Hueter from Marburg, Germany. The approach was then popularised in the fifties of the past century by the Judet brothers in Paris. The approach is therefore by some also unfairly called the ‘French’ approach
Currently, Stephan Vehmeijer places hip prostheses in all patients, without exception, through the anterior approach. Over the years, he has further improved the approach to reduce blood loss during surgery and to make even less damage. Incidentally, this does not mean that things always go smoothly after surgery in all patients. It really is still a major surgery.
However, after the anterior approach, compared to other approaches, patients have demonstrably less pain in the first period after surgery and need a shorter period to walk with crutches. Nine years after surgery, patients operated via the anterior approach have a (limited) lower risk of needing a second operation than patients operated via the posterior approach. This is mainly because the risk of hip dislocation is slightly higher in the posterior approach.
Robot-assisted surgery
At the ReinierHaga Orthopedic Centre, Stephan Vehmeijer also performs surgery with the help of a MAKO robot. The advantage of surgery with the help of the robotic arm is that the hip can be placed very precisely. In fact, the robot guides the orthopedist to place the prosthesis exactly as determined by a CT scan before the operation. The disadvantage of robot-assisted surgery is that an additional incision of about 4 cm must be made over the iliac crest. This is necessary because pins need to be inserted here so that the robot can determine the precise position of your pelvis.
A second drawback is that a CT scan of the hip must be made prior to surgery. You will have to come to the hospital for this. A third drawback is that surgery takes approximately fifteen minutes more in total.
Research from 2022 shows that, for now, the results of robot-assisted surgery are equivalent to surgery via the anterior approach using X-ray guidance (Stephan Vehmeijer’s standard method of surgery).

Revision total hip replacement
Of course, there are always exceptions, but in almost all cases a second (or third) surgery on an artificial hip can also be performed via the anterior approach. Stephan Vehmeijer has extensive experience with this type of surgery and also gives courses for the technique internationally. This type of surgery is exclusively performed at the ReinierHaga Orthopedic Centre in Zoetermeer. Please contact this centre for further information.